January 16, 2026 – A new study reveals that bacteria can survive antibiotic treatment through two fundamentally different modes, resulting in antibiotic persistence, a major cause of treatment failure and difficulty in curing.
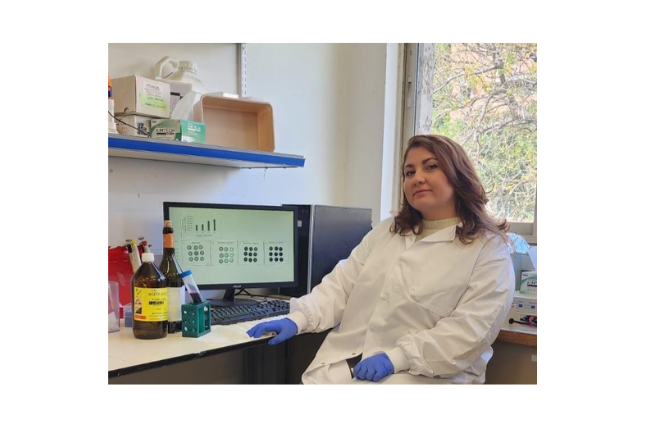
For years, persistence has largely been blamed on bacteria that shut down and lie dormant, essentially going into a kind of sleep that protects them from antibiotics designed to target active growth. But a new study published in Science Advances led by Ph.D. student Adi Rotem under the guidance of Prof. Nathalie Balaban from the Hebrew University of Jerusalem (HU) reveals that this explanation tells only part of the story.
“We found that bacteria can survive antibiotics by following two very different paths,” said Prof. Balaban. “Recognizing the difference helps resolve years of conflicting results and points to more effective treatment strategies.”
Antibiotics are prescribed for a wide range of indications, from chronic urinary tract infections to infections tied to medical implants. Yet in many stubborn infections, a small number of bacterial cells manage to survive, only to re-emerge later and cause relapse. This phenomenon, known as antibiotic persistence, is a significant contributor to treatment failure and one reason infections can be so difficult to fully cure.
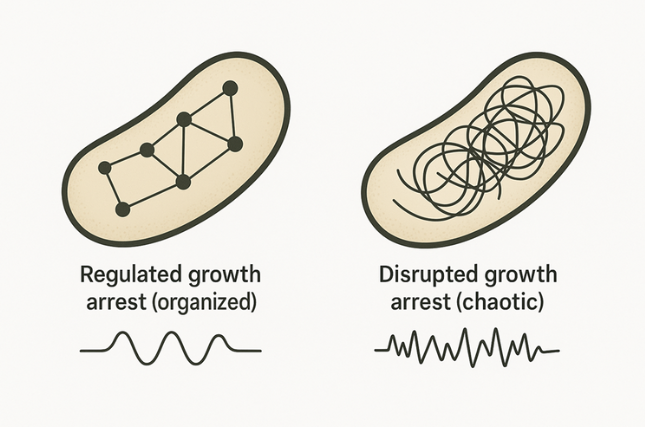
The study shows that high survival under antibiotics can originate from two fundamentally different growth-arrest states, and they are not just variations of the same “sleeping” behavior. One is a controlled, regulated shutdown, the classic dormancy model. The other is something entirely different: a disrupted, dysregulated arrest, where bacteria survive not by protective calm but by entering a malfunctioning state with distinct vulnerabilities.
How the Researchers Saw What Others Missed
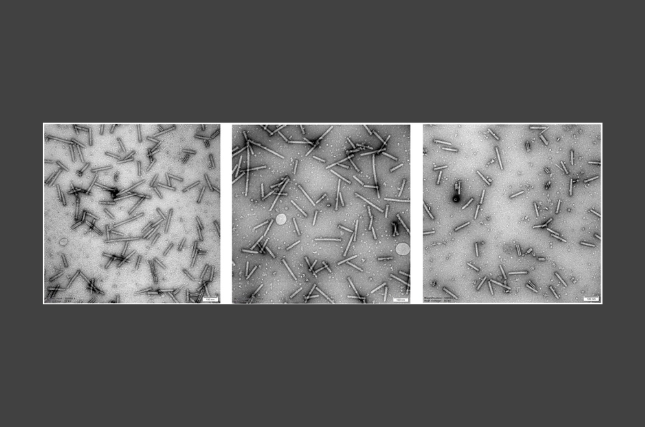
The team combined mathematical modeling with several high-resolution experimental tools, including:
- Transcriptomics, to measure how bacterial gene expression shifts under stress
- Microcalorimetry, to track metabolic changes through tiny heat signals
- Microfluidics, allowing scientists to observe single bacterial cells under controlled conditions
A Framework That Could Transform Antibiotic Strategies
Despite intense research, scientists have struggled to agree on a single mechanism explaining why Persister cells survive. Different experiments have produced conflicting results about what Persisters look like and how they behave. This study explains: researchers may have been observing various types of growth-arrested bacteria without recognizing they were distinct.
By separating persistence into two different physiological states, the findings suggest a future where treatments could be tailored, targeting dormant Persisters one way, and disrupted Persisters another.
Together, these approaches revealed clear biological signatures distinguishing regulated growth arrest from disrupted growth arrest, along with the specific vulnerabilities of the disrupted state.
Funding for the study was provided by the European Research Council Advanced Grant, grant no. 101054653, The Minerva Center for Stochastic Decision Making in Microorganisms, Israel Science Foundation grant no. 597/20 and the Milner Foundation, founded by Yuri Milner and his wife Julia (AR).
The research paper titled “Differentiation between regulated and disrupted growth-arrests allows tailoring of effective treatments for antibiotic persistence” is now available in Science Advances and can be accessed here.
Researchers:
Adi Rotem1, Yoav Kaplan1, Orit Gefen1, Irine Ronin1, Alon Gutfreund1, Hagai Rappeport1, Raya Faigenbaum-Romm1, Nitsan Naor1, Elisheva Stav1, Oded Agam1, Nathalie Q. Balaban1
Institutions:
- Racah Institute of Physics, The Hebrew University of Jerusalem