July 2, 2025 – SARS-CoV-2 protein can spread from infected to uninfected cells, triggering an immune response that mistakenly targets healthy cells, according to a new study by researchers from the Hebrew University of Jerusalem.
Published in Cell Reports, this research uncovers a surprising way in which the SARS-CoV-2 virus can misdirect the immune system, causing the attack of healthy cells, simply because they have been marked by a viral protein. Understanding this mechanism opens the door to new strategies for preventing inflammation and cellular damage that might contribute to severe COVID-19 outcomes and complications such as long COVID.
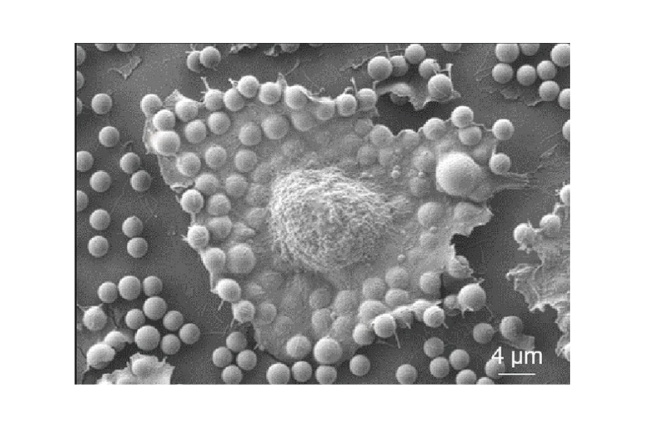
The study demonstrates that the SARS-CoV-2 nucleocapsid protein (NP) is transferred to neighboring uninfected epithelial cells and attaches to their surfaces. NP is recognized by the immune system of these otherwise healthy cells and is targeted by anti-NP antibodies, which mistakenly label the cells for destruction.
The research was led by Ph.D. students Jamal Fahoum and Maria Billan from the Hebrew University Faculty of Medicine. They also found that the drug enoxaparin, a commonly used blood thinner, can block the viral protein from sticking to healthy cells. It does this by taking over the spots the protein would normally bind to, as a heparin analog, which mimics heparin. Both lab experiments and patient samples showed that enoxaparin stopped the protein from attaching to cells and helped prevent the immune system from mistakenly attacking them.
The SARS-CoV-2 infection experiments were performed in the recently established high biocontainment national laboratory, Barry Skolnick Biosafety Level 3 National Research Laboratory (BSL3) at the Core Research Facility at the Faculty of Medicine at Hebrew University.
The study was supported by several research funds, including major contributions from The Edmond and Benjamin de Rothschild Foundation and The Israel Science Foundation of the Israel Academy of Science and Humanities.
The research paper titled “Transfer of SARS-CoV-2 nucleocapsid protein to uninfected epithelial cells induces antibody-mediated complement deposition” is now available in Cell Reports and can be accessed here.
Researchers:
Jamal Fahoum1,2,13, Maria Billan2,3,13, Julia K. Varga2,14, Dan Padawer2,4,14, Yelena Britan-Rosich5,14 Maya Elgrably-Weiss2, Pallabi Basu2,6, Miri Stolovich-Rain2,3, Leah Baraz2,3,7, Einav Cohen-Kfir1, Sujata Kumari1,2,3, Esther Oiknine-Djian 8, Manoj Kumar1, Orly Zelig9, Guy Mayer10, Michail N. Isupov11, Dana G. Wolf8,12, Shoshy Altuvia2, Reuven Wiener1,Ora Schueler-Furman2, and Alexander Rouvinski2,3,15
Institutions:
- Department of Biochemistry, Institute for Medical Research Israel-Canada, The Hebrew University-Hadassah Medical School, The Hebrew University of Jerusalem
- Department of Microbiology and Molecular Genetics, Institute for Medical Research Israel-Canada, The Hebrew University-Hadassah Medical School, The Hebrew University of Jerusalem
- The Kuvin Center for the Study of Infectious and Tropical Diseases, The Hebrew University-Hadassah Medical School, The Hebrew University of Jerusalem
- Institute of Pulmonary Medicine, Hebrew University-Hadassah Medical Center
- Barry Skolnick Biosafety Level 3 (BSL3) Unit, Core Research Facility, Faculty of Medicine, Hebrew University of Jerusalem
- Dove Laboratory, Boston Children’s Hospital
- Department of Medical Laboratory Sciences, Jerusalem Multidisciplinary College
- Clinical Virology Unit, Hadassah Hebrew University Medical Center, Israel Hadassah Hebrew University Medical Center
- Blood Bank, Hebrew University-Hadassah Medical Center
- The Institute of Chemistry, The Hebrew University of Jerusalem
- The Henry Wellcome Building for Biocatalysis, Biosciences, University of Exeter
- Lautenberg Centre for Immunology and Cancer Research, The Institute for Medical Research Israel-Canada (IMRIC), Faculty of Medicine, Hebrew University of Jerusalem