June 25, 2025 – When people experience short-term (acute) pain, the brain has a built-in way to dial down pain signals—like pressing the brakes—to keep them from going into overdrive, which differs from long-term (chronic) pain, according to new findings by researchers from the Hebrew University of Jerusalem (HU).
According to the study published in Science Advances, researchers reveal that our bodies respond to acute (short-term) and chronic (long-lasting) pain in surprisingly different ways at the cellular level. Their discovery sheds new light on how pain becomes chronic and opens the door to better-targeted treatments. Chronic pain affects over 50 million people in the U.S. alone, often with few effective treatment options.
“This is the first time we’ve seen how the same neurons behave so differently in acute versus chronic pain,” said Professor Alexander M. Binshtok from the Hebrew University-Hadassah School of Medicine and HU’s Edmond and Lily Safra Center for Brain Sciences (ELSC), who supervised doctoral student Ben Title. “The fact that this natural ‘calming’ mechanism is missing in chronic pain suggests a new target for therapy. If we can find a way to restore or mimic that braking system, we might be able to prevent pain from becoming chronic.”
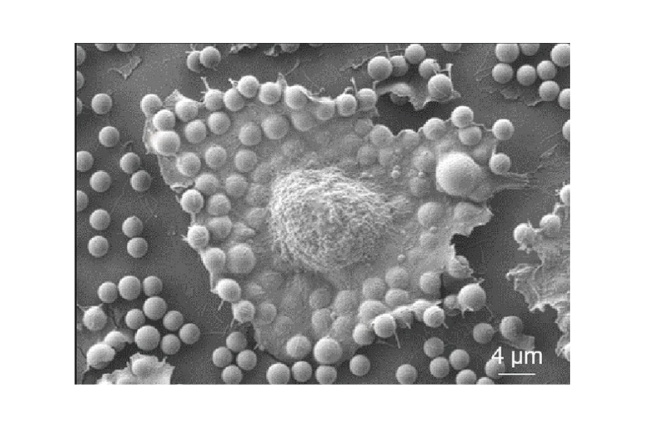
This new study adds an important piece to the puzzle by showing how the nervous system’s built-in pain controls are disrupted in long-term pain conditions. The team studied a small but crucial region in the brainstem called the medullary dorsal horn, home to neurons that act as a relay station for pain signals. These projection neurons help send pain messages from the body to the brain.
During acute inflammatory pain, these neurons help limit the number of pain-related signals sent to the brain. Once the inflammation and pain subside, the neurons return to their normal state. However, during chronic pain, the neurons become more excitable and fire more signals, potentially contributing to the persistence of pain.
Using a combination of electrophysiology and computer modeling, the researchers identified a key mechanism: a specific potassium, currently known as the A-type potassium (IA). This current helps regulate the excitability of neurons.
In acute pain, IA increases, acting like a natural sedative for the pain pathways.
By understanding the brain’s own strategies for limiting pain—and why they sometimes fail—scientists are now one step closer to developing smarter, more precise therapies for those who suffer from chronic pain.
The research paper titled “Opposite regulation of medullary pain-related projection neuron excitability in acute and chronic pain” is now available in Science Advances and can be accessed here.
Researchers:
Ben Title1,2, Enrique Velasco1,3,4, Nurit Engelmayer1,2, Prudhvi Raj Rayi1,2, Roy Yanai1,2, Shmuel Hart1,2, Ben Katz1,2, Shaya Lev1,2, Yosef Yarom2,5 and Alexander M Binshtok1,2
Institutions:
1. Department of Medical Neurobiology; Institute for Medical Research Israel-Canada, The Hebrew University-Hadassah School of Medicine
2. The Edmond and Lily Safra Center for Brain Sciences, The Hebrew University of Jerusalem
3. Department of Cellular and Molecular Medicine, KU Leuven; VIB Center for Brain and Disease Research
4. Neuroscience in Physiotherapy (NiP), independent research group
5. Department of Neurobiology, The Alexander Silberman Institute of Life Sciences, The Hebrew University of Jerusalem